It's been a while since I've given a good update on where we're at with Luke's heart. As you know, Luke has AV Canal and he is facing open heart surgery. The repair for this particular defect generally occurs when the individual is between 4 and 6 months old... Luke is currently 18 weeks, which puts him 2 weeks shy of 4 months.
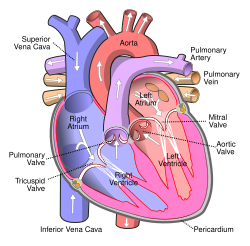
We've been hoping at our last few cardiology visits to get an estimation on timing for the repair, however with each conversation, we've heard different time frames. Before he was born, we heard that it would be between 4-6 months old. After he was born and was still in the NICU, we were hearing that it could be around when he was 6 months old, mostly because of issues like his Patent Ductus Arteriosis (PDA) taking a while to close after he was first born. Then he contracted the RSV virus and once he'd recovered from RSV, we heard that it could be as late as when he's 18-24 months old. I don't necessarily think that him getting RSV changed anything for him, I think it was more related to him getting bigger and stronger and his heart dealing with the defect better as he's continued to grow. As a generalization, what we've heard has been that overall he presents well and the blood pressure in his lungs is at an acceptable level. Not to go into the blood pressure thing too much because I still don't fully understand all of the complexities, but basically, the heart is a pump. The right side of your heart receives blood from the body and pumps it to the lungs. The left side of the heart does the exact opposite: It receives blood from the lungs and pumps it out to the body. The two holes in Luke's heart allow a portion of the oxygenated blood from left side of the heart to flow back into the right side where it mixes with the de-oxygenated blood and is re-pumped to the lungs. If left untreated for too long, the increased blood flow aka blood pressure will cause the right side of the heart and lungs to become enlarged... an irreversible problem that would lead to additional life long cardiology and pulmonary problems. If left completely untreated, Luke would probably not live past childhood or at the longest, through adolescence, versus with the repair, his life expectancy should increase to at least 50 years old. At our last cardiology appointment, we did our routine visit, one that consists of an echocardiogram, which is basically an ultrasound of the heart, he had an electrocardiogram, which is where they place little stickers on his chest that connect wires to a computerized machine that measures his heart rhythm and he also had his blood pressure measured in all four extremities as well as the usual weight, length and pulse ox measurements. Everything looked good, with the exception of there being some ambiguity when the results were read of the echo as the hole between Luke's ventricular chambers of his heart (this particular part of the defect is known as the VSD) is structurally located close to his tricuspid valve. Apparently when reading the echo, it was hard to determine where the blood flow that they could visualize was coming from... was it from the tricuspid valve which would be normal or was it coming from the VSD? If the flow is coming from the VSD, surgery would be required sooner rather than later.
In response, our cardiologist has recommended that Luke undergo a sedated echocardiogram, which they are hoping will allow them to get a better ultrasonic view of his heart. This means that he will be under anesthesia and will also be intubated and breathing on a ventilator while they perform the echo. Our doctor hopes that with him being completely still they will be able to see what they need... supposing they don't see what they need, while he is all set up on the vent and anesthesia, they will continue with a heart catheterization. If they proceed with doing the heart cath, they will no doubt find what they need as it would be an invasive procedure, similar to what is done with adults. With a heart cath they will place a catheter through the femoral artery in the groin area and proceed to the heart where they will be able to accurately measure the amount of flow coming across the VSD, the blood pressures in the heart and will also inject dye through the catheter and will take x-ray video to record where and how liquid flows through the heart and lungs.
The procedure is scheduled for coming Thursday morning - we have to be at the Clinic by 7 AM and it sounds like they hope to be starting with him by 8 or 8:30. Apparently, if they only need to do the echo, he should be done by 9:30 or 10 and if they end up also doing the cath, that will add another 2 hours to the procedure. The benefit for us will be that once they're done, we will have word from our cardiologist of what they found and a good idea of when they will be scheduling his open heart surgery. I think we will be able to be with him right up until he is taken to the pediatric cath lab and will also get to see him again once he is in recovery and will hopefully be there to greet him as he wakes up from the anesthesia.
As I've been thinking about this and counting down the days until we mentally and physically move into the very draining "Clinic" mode, which has historically included time in the NICU, washing clothes at the Ronald McDonald Family Center, preparing for our doctor's rounds and discussing medical terminology I don't fully understand, I have decided to just cherish every moment with our boys over the next few days. The sedated echo and heart cath are pretty routine procedures and our doctor has indicated there is a less than 1% risk associated with them being performed. We don't expect for Luke to be in the hospital long and we already have family care lined up for Matthew which will allow him to stay in his surroundings and sleep in his own bed, minimizing any impact to his own routine and further eliminating worry from mine and Dustin's minds as to where he is and what he's doing. Before giving Luke his bath last night, I decided to capture a few moments with our sweet little man.




No comments:
Post a Comment